As the omicron variant of the coronavirus spreads in Alaska, state public health officials say their systems for monitoring and responding continue to adapt to the latest science, the needs of Alaskans and the resources available. Deciding to end free, COVID-19 lab tests for travelers at airports was just one piece of that.
It’s part of a wider push to use more rapid, at-home test kits in general, which impacts other public health systems officials have been using to manage the pandemic.
“And so this is part of communicating and sharing with the public the transition that we are going through,” said Heidi Hedberg, the director of the state’s Division of Public Health.
She used the word “transition” seven times during our interview.
The upshot of home rapid tests is they’re faster, more convenient and much less expensive than lab tests. Hedberg said the cost of a lab test works out to about $62, while a two-test antigen kit costs between $15 and $25.
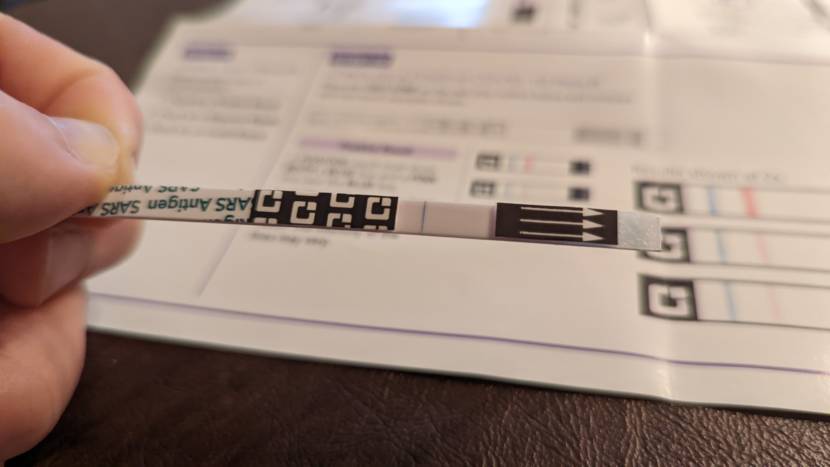
The downside is that these tests, also referred to as antigen tests, aren’t as sensitive. So you’re really supposed to use both tests in a given kit over 36 hours to be confident about a negative result.
Also, Hedberg said there’s no built-in way for the state to find out if one of these tests comes out positive; a case caught through a home test is only captured in the state’s pandemic data if it’s voluntarily reported.
That means case count data won’t necessarily be complete. But state epidemiologist Dr. Joe McLaughlin said lab tests aren’t going away, which do feed into state case counts. That data is still valuable to track case trends over shorter periods of time.
To assess risk, there is other data, which the state intends to keep reporting three days a week.
“The data on hospitalization and death really won’t change,” McLaughlin said. “That will still be robust data that we will still use to help also monitor morbidity and mortality rates.”
In Juneau, for example, the head of the city’s pandemic response, Robert Barr, said he’s putting more weight on how burdened the medical system is. Early on in the pandemic, high case counts necessarily meant higher hospitalizations and deaths. But at this point, more effective treatments are available, and vaccines and prior infections mean there are fewer severe cases.
In other words, communities can tolerate higher case counts now than they could in 2020.
The convenience of home test kits also comes with the responsibility of tracing one’s own contacts.
“We’re really relying heavily on Alaskans to do the right thing, with respect to self-isolation if you’re positive, following the guidance there,” McLaughlin said. “And then notifying their own close contacts if they do come up positive so that those close contacts can appropriately quarantine if they’re unvaccinated.”
The supply of home tests has shot up over the last year, but so has demand.
“But we also know that there’s going to be limited supply chain constraints on occasion,” Hedberg said. “You know, that’s just part of this pandemic and what we have been experiencing over the past two years. … I anticipate that that’s going to continue in 2022.”
Hedberg said retailers also have home kits for sale, and more market options may be coming.
“We’ve heard from a lot of the private sector that they’re really interested in really establishing their own business and offering these antigen tests at low cost,” Hedberg said. “Which is really great, from a public health standpoint. We want to ensure that there is access to testing.”
Meanwhile, the total confirmed count of COVID-19 cases caused by the fast-spreading omicron variant in Alaska is up to six, as of Tuesday afternoon.
“We’re bracing for an omicron wave,” McLaughlin said. “Many states in the U.S. are already dealing with a substantial omicron wave. … Our hope is to get through that wave as quickly as we can. The best way to prepare for it is to get vaccinated if you’re not already vaccinated. To get boosted, get a booster dose of the vaccine if you’re eligible.”
Health authorities say that vaccination and prior infection aren’t proving as effective at preventing infection from this variant, but they do still appear to protect against severe illness.
“People need to be pretty vigilant about masking, social distancing, avoiding crowds. I would say even more vigilant than we were with other variants,” McLaughlin said.
He said it’s also time to step up our masking practices.
“With masking, probably just a single-layer cloth face covering is not going to be good enough to help prevent infection,” McLaughlin said. “It might help a little bit, certainly when somebody is coughing or sneezing, it really does stop those larger respiratory droplets from getting out into the air. But it’s better to have a two-ply mask.”
McLaughlin said it’s important that masks fit well. The better the fit, the better the filtration. For crowded, high-risk situations, McLaughlin recommended N95 respirators, which are no longer in short supply.
There have been some indications that the omicron variant may be less dangerous than earlier variants. But McLaughlin said it’s too soon to conclude that.
“Some of the studies coming out of South Africa suggest that it may be a milder illness,” he said. “Some of the early studies out of the U.K. and Denmark suggest that it might actually be roughly equivalent to delta, with respect to hospitalization rates. So at this point, it’s really just too early to say. There are too many variables that really haven’t been teased out in the epidemiologic studies.”
At some point, McLaughlin said these coronaviruses will eventually become endemic.
“It will be a part of the whole group of respiratory viruses that we deal with on a regular basis. … We will eventually develop such a high level of prior immunity through vaccination and through prior infection, the virus will likely continue to morph and change over time,” he said. “The hope is that it changes in the direction of becoming less and less virulent over time.”
But for the foreseeable future, McLaughlin and Hedberg said the state’s emergency management systems are not scaling back, just transitioning.